Pulmonary Hypertension: Overview
This information was reviewed and approved by Marjorie Patricia George, MD (1/31/2020).
Pulmonary hypertension is a condition of high blood pressure in the blood vessels of the lungs. Normally, venous (low oxygen) blood returns from the body to the right side of the heart. When people have pulmonary hypertension, they develop shortness of breath, fatigue, and swelling, among other symptoms. It is important to make an early and accurate diagnosis to be able to treat it and help people breathe better.
Pulmonary hypertension is high blood pressure in the arteries of the lungs and it makes people short of breath.
There are five different categories of pulmonary hypertension. The first type is pulmonary arterial hypertension, which is a disease of the arteries of the lungs themselves. The second type is pulmonary hypertension due to heart disease. The third type is pulmonary hypertension due to lung disease or in chronic low oxygen levels or sleep apnea. The fourth type is pulmonary hypertension due to chronic blood clots in the lungs. And the fifth type is pulmonary hypertension due to miscellaneous diseases.
Early pulmonary hypertension is manifest with shortness of breath when someone exerts themselves. As it progresses, people can do less and less in terms of an activity tolerance. As the disease progresses, people may develop swelling in their lower extremities or even in their abdomen.
Making the diagnosis of pulmonary hypertension can be challenging because it looks like a lot of other diseases. Oftentimes people are misdiagnosed with asthma or COPD or obesity or just being out of shape. It's really important to make an accurate diagnosis and the gold standard test to making the diagnosis is a right heart catheterization.
The goals and treatment of pulmonary hypertension are for us to make an early diagnosis. So number one, it's important to, when it's suspected, do the appropriate testing so that we can make an early diagnosis in this disease. And then we treat it aggressively. We have medications available and our goals are to help the patient breathe better, walk further, do more and live longer.
Classifications of Pulmonary Hypertension
There are five different types of pulmonary hypertension (PH). These types are categorized into groupings based on the causes and treatments of the disease. The groups are known as the World Health Organization (WHO) classification system.
WHO Groups of Pulmonary Hypertension
| Group | Name | Caused by | Risk Factors |
| 1 | Pulmonary Arterial Hypertension (PAH) —due to a disease of the arteries themselves | Increased stiffness, narrowing or scarring of the pulmonary arteries stresses the heart, losing its ability to pump enough blood through the lungs. |
|
| 2 | PH Due to Left Heart Disease — heart failure or heart valve problems | The left side of the heart does not pump correctly, creating a back pressure into the lungs. |
|
| 3 | PH Due to Chronic Lung Disease and Hypoxia (low oxygen levels) including Sleep Disorders | Shortage of oxygen causes the arteries in the lungs to tighten. |
|
| 4 | PH Due to Chronic Arterial Obstructions — blockages in the pulmonary arteries | Blood clots that the body can’t dissolve or other obstructions block pulmonary arteries. |
|
| 5 | PH from Unknown Causes | Not well understood. |
|
As the chart below shows, most patients are diagnosed with PH due to left heart disease (Group 2) and/or PH due chronic lung disease with low oxygen levels, Group 3.
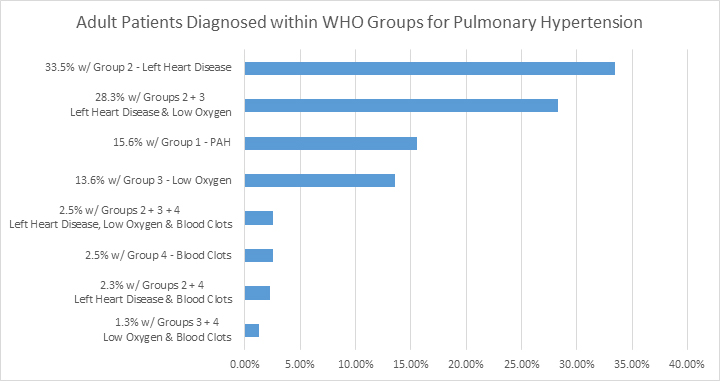
Chart source: Wijeratne, D. T., et al. (2018). Increasing Incidence and Prevalence of World Health Organization Groups 1 to 4 Pulmonary Hypertension: A Population-Based Cohort Study in Ontario, Canada. Circulation. Cardiovascular Quality and Outcomes, 11(2), e003973.
Associated Conditions
Pulmonary hypertension can occur in isolation or, more commonly, with diseases of the lungs and heart. Pulmonary hypertension in the absence of other diseases is very rare and is often idiopathic, associated with autoimmune disease or familial in nature. This kind of pulmonary hypertension is referred as pulmonary arterial hypertension (PAH). Pulmonary arterial hypertension can also be associated with drug use, such as methamphetamines or diet drugs; human immunodeficiency virus (HIV); liver disease; and congenital heart disease.
Pulmonary hypertension is commonly associated with a variety of lung conditions. These include COPD, emphysema, interstitial lung disease, chronic pulmonary blood clots or untreated sleep apnea. When pulmonary hypertension arises from cardiac conditions such as heart failure or heart valve disease, it is sometimes referred to as pulmonary venous hypertension. And while there are specific types of pulmonary hypertension, it is important to note that pulmonary hypertension can be associated with multiple causes.
See how your heart can affect your breathing in our infographic explaining the heart/lung connection.
Learn about the Pulmonary Hypertension Program at National Jewish Health.
Pulmonary Hypertension: Symptoms
Healthy pulmonary arteries of the lungs are elastic. They expand and contract with each beat of the heart. In pulmonary hypertension, arteries stiffen and thicken. This leads to increased resistance to blood passing through the vessel, thereby increasing pressure. Higher pulmonary pressure can lead to symptoms of pulmonary hypertension. These symptoms can involve the heart.
View Do I Have High Blood Pressure in My Lungs Infographic
Common symptoms of pulmonary hypertension may include:
• Shortness of breath, especially with exertion
• Fatigue
• Low oxygen levels
• Chest pain or pressure
• Near-fainting/fainting
• Palpitations
• Swelling of the ankles or abdomen
• Heart failure (in advanced cases).
Pulmonary Hypertension: Diagnosis
Because the symptoms of pulmonary hypertension can look like symptoms of more common diseases (e.g., COPD, asthma, sleep apnea), the diagnosis of pulmonary hypertension can be challenging and is often delayed until the disease has progressed.
When suspecting pulmonary hypertension, the first step is getting an ultrasound of the heart, or echocardiogram, which can provide an estimate of the pressure in the lungs.
Only a procedure called a right heart catheterization (RHC) can directly measure blood pressure in the lungs and determine if pulmonary hypertension is present. Doctors use the pattern of numbers from the heart catheterization, along with the patient’s other testing, to determine whether the patient has pulmonary hypertension, and if so, what type. This helps determine the best course of therapy for each patient.
Other tests are performed to look for associated diseases, including blood tests, electrocardiogram (EKG), chest X-ray, pulmonary function tests and a test for chronic blood clots in the lung called a ventilation/perfusion scan (VQ scan). A six-minute walk time is typically performed to assess a person’s exercise capacity and need for oxygen therapy. It is also important for patients to have a sleep study or a nighttime oxygen test.
While the testing can be intensive, especially at the time of diagnosis, these data are essential to mapping out a personalized plan to help the patient with pulmonary hypertension live and breathe better.
Pulmonary Hypertension: Treatment
Treatment of pulmonary hypertension is directed toward improving your symptoms and ability to move; delaying progression of the disease; and, most important, helping you have a better quality of life. The treatment used for pulmonary hypertension depends upon its underlying cause.
Non-medication Treatments for Pulmonary Hypertension
Important non-medication treatment includes:
• Removal of harmful drugs
• Healthy nutrition, consisting of real food, low in sodium and sugar (especially if there are issues with fluid retention)
• Routine exercise (with the guidance of your pulmonary hypertension doctor).
Medication and Other Treatments for Pulmonary Hypertension
People whose pulmonary blood pressure “responds” to inhaled vasodilator treatment during right heart catheterization may be candidates for calcium channel blocker therapy. People with pulmonary arterial hypertension (PAH) that does not respond to vasodilator challenge during right heart catheterization or who do not improve with calcium channel blocker treatment, or people who have inherited, or connective tissue-associated pulmonary hypertension, or PAH due to other causes may be candidates for vasodilator therapy.
Pulmonary hypertension medications come in different forms: oral, inhaled, intravenous (through an IV catheter) and subcutaneous.
Pulmonary hypertension medications include:
• Phosphodiesterase-5 (PDE-5) inhibitors (sildenafil or tadalafil)
• Soluble guanylate cyclase stimulator (riociguat)
• Endothelin receptor antagonists (ERAs) (bosentan, ambrisentan, macitentan)
• Prostacyclin pathway medications (epoprostenol, treprostinil, selexipag).
Medications in the prostacyclin pathway may improve symptoms, exercise tolerance and sometimes survival. These medications can be given orally (selexipag, treprostinil); by inhalation (treprostinil); by subcutaneous injection (treprostinil); or via IV infusion (epoprostenol, treprostinil). While these medications can provide significant improvement, they require judicious dosing and have many side effects. They should be managed at pulmonary hypertension programs experienced with their use.
In treating pulmonary arterial hypertension, patients are often started on multiple medications at the same time or in rapid succession to target multiple pathways in this disease and achieve the best response in the shortest amount of time.
In people who have pulmonary hypertension due to chronic blood clots, known as chronic thromboembolic pulmonary hypertension (CTEPH), surgical removal of the scar tissue or balloon pulmonary artery angioplasty is always considered, as this can be of greatest benefit. In patients with CTEPH, lifelong treatment with a blood thinner is crucial to prevent more blood clots.
When pulmonary hypertension develops into heart failure, diuretics, digoxin and sodium restriction can be helpful.
Finally, lung or combined heart/lung transplantation may be appropriate in people who have progressive disease and in whom medical therapy has failed.
 Clinical Trials
Clinical Trials
For more than 100 years, National Jewish Health has been committed to finding new treatments and cures for diseases. Search our clinical trials.
